|
The History of General Practice in Australia
Please note that this page is very much a work in progress.
Australia's First Medicine Men
Australia's first medicine men of course were
the Aboriginal medicine men. At the time that James Cook arrived in
Austalia (1760) it is likely that the Australian traditional healers
were better at treating their patients than the English doctors were at
treating theirs. Both could set broken bones and treat wounds tolerably
well. To the English, diseases were due to miasmas (mysterious odours
coming from decaying material), diseased parents, sedentary habits,
emotional upset or environmental conditions such as getting cold or wet.
They had essentially no effective treatments for medical problems. The Aboriginal medicine
man saw disease as a disturbance of the patient's spirit and sought to
rectify that disturbance. The Aboriginal doctor had a large
pharmacopoeia of active drugs at his disposal (of herbal and animal orgigin). The English doctor had
but a handful of drugs that actually worked, and only one of those
(quinine) was of any use in infectious diseases (malaria) unless one
considers the widespread use of mercurial salts for syphilis as being
useful.
A further account of the Australian traditional healer can be read here.
The Practice of Medicine in Early England
"The present classification of medical men
is a child of circumstances. In former ages, nay, even within the last
three centuries, there really was but one species of practitioner in
this country. This was the physician; for, although persons practicing
surgery existed before that period, they were a degraded race of men as
far as medicine is concerned. They were only persons exercising the
calling of barbers, who took upon themselves to bleed and draw teeth; to
perform other slight operations in surgery, and ultimately to engage in
the medical care of surgical diseases. Hence gradually arose a
corporation of barber-chirurgeons, and after a time of division of this
corporation and the institution of a new one, under the name of
Corporation of Chirurgeons.
With respect to physicians, it is probable
also that they were at first apothecaries or shopkeepers; that is to
say, they dispensed their own medicines. After a time, however, it
became convenient that a separate class of apothecaries should be
formed. But the physician tried to take special care that the apothecary
should be confined to his own calling, and on no account engage in the
practice of medicine. The apothecary, then, held the same situation that
appertains, or ought to appertain, to the present druggist.
Nevertheless, public convenience, which sets at defiance the private
interests of individuals or sets of individuals, called on the
apothecary to prescribe, as well as to dispense medicine. The physicians
took fire at this, and a most virulent and entertaining war took place
about two hundred years ago, between the physician and the apothecary;
the former being actuated by the vain hope of preventing the latter from
obeying the commands of a far superior power. Of course the physician
failed in his object; the apothecary became established as a regular
practitioner; the wants of society, if not the law, sanctioned his
existence, and hence arose the general practioner.
The world never stands still; and as society
in this country did not retrograde, its wants and its improvements went
hand in hand, until at last the general practitioner became so
extensively engaged in the practice of medicine, that a further division
was found to be convenient, and about thirty years ago, the new order
of druggists arose."
Taken from the Transactions of the Associated Apothecaries and Surgeon- Apothecaries, 18238. |
It should be understood that in England and
particularly London, occupations were controlled by livery companies
(guilds and trade associations) that had features of professions, trade
unions and secret societies. These companies controlled the
trades/professions partly by regulating membership. The practice of
medicine in the era before England colonised Australia was controlled by
three groups:
- The surgeons
- The physicians
- The apothecaries
 |
The surgeons
had their origins with the Guild of Surgeons Within the City of London
in the 14th century. Prior to this, monks were the traditional healers,
however a papal decree forbad them to shed blood. The barbers assisted
the monks and were to perform blood-letting, leeching, drainage of
abscesses, extraction of teeth, enemas, fire cupping, leeching, neck
manipulation, as well as hair cutting and shaving.
In 1462 the Worshipful Company of Barbers was incorporated. There was
a conflict between the surgeons and the barber surgeons until an
agreement in 1493 was signed giving the surgeons the power of
incorporation. They became the Guild of Surgeons. Henry VIII ratified a
combining of the two to become the Company of Barber Surgeons in 1540.
In 1745 the surgeons requested a separation and this was granted by an
act of parliament. They formed the Company of Surgeons. They built a new
hall with an anatomy theatre near Newgate Gaol so it could dissect the
bodies of executed criminals for learning and teaching purposes. In 1800
they became the Royal College of Surgeons (RCS). Although this was
changed to the Royal College of Surgeons of England in 1843, it remained
commonly known by its former name.
|
Because they did not have a formal university education, the surgeons
were not givern the title "Dr", a custom which persists today. 1843
also saw the formation of the higher qualification, the Fellowship of
thge Royal College of Surgeons (FRCS). From the 1800s the examinations
were held in conjunction with the Royal College of Physicians and those
who passed were given the post-nominal, MRCS LRCP (Member of the Royal College of Surgeons, licentiate of the Royal College of Physicians).
| The physicians.
The College of Physicians of London (also known as the King's College)
was founded by royal charter (King Henry VIII) in 1518, following a
petition led by Thomas Linacre. The purpose of the petition was to seek
recognition of trained physicians to distinguish them for the untrained
practitioners that practiced under the same nomenclature. The College's
powers were extended from London to the rest of England in 1523 by an
act of parliament. It became known as the Royal College of Physicians
(RCP)in the 17th century following the re-establishment of the monarchy.
Initially the training was academic and required a demonstrated
classical education as well as an education in medicine. Examinations were viva
voce. There were fewer than sixty fellows (and 100 licentiates) at any
time up until the 19th century. One issue of contention was the
admission to the College of non-Oxbridge trained practitioners. |
 |
It was not until 1835 that practitinoers from other universities
were allowed fellowship. Similarly membership excluded women until 1909.
The College published the London Pharmacopoeia in 1618 and this was the first standardised list of medications in England. In 1869 it also published the Nomenclature of Diseases, which became an international standard for naming diseases until the 20th century.
The College previously issued a Licentiate of the Royal College of
Physicians (LRCP), available to Oxbridge medical graduates. This
post-nominal was ceased in 1999. Those passing the RCP examinations were
became Fellows (FRCP).

|
The apothecaries
were descended from the grocers (so named because they bought in
gross quantities). The Grocer's Company was described in 1365 as the "Mistery of
Grossers, Pepperers and Apothecaries". One can imagine that the
apothecaries were those who specialised in the trade of items of
medicinal use. Over time they became the experts in the use of the
substances they traded. Consequently they sought to become a guild of their
own. In 1617 they were granted a royal charter by James I and formed the Worshipful Society of Apothecaries. They challenged the College of Physicians regarding their monopoly in practicing medicine.
|
In 1673 the Society created the Chelsea Physic Garden
(which still exists). This was a place where medicinal plants were
grown and studied. The garden was used to teach medical students botany.
It became one of the most important centres for botany and plant
exchange in the world.
In 1704 the "Rose Case" was a landmark trial. The House of Lords
overturned a prior ruling of the Bench of the Queen and allowed Thomas
Rose (an apothecary) to prescribe. This was seen as a license for all apothecaries to
prescribe. However, they were not allowed to charge for their diagnostic
services, but were only allowed to charge for the medications they
provided. The apothecaries were, therefore allowed to practice medicine.
In 1815 the Apothecaries Act was to give the Society power to license
and regulate medical practitioners throughout England and Wales. It
continued to do this until 1999 (when the Uniting Examination Board was
disbanded). The Society of Apothecaries went on to liaise with the
College of Physicians and eventually together with the College of
Surgeons form conjoint examining bodies for the purpose of registering
medical practitioners. A qualification through the Society of
Apothecaries was the LSA (Licentiate of Apothecaries).
In recent times (1928 - 2002) the Society of Apothecaries offered diplomas in areas not covered by the colleges:
- the Mastery of Midwifery (MMSA)
- Diploma in the Forensic and Clinical Aspects of Sexual Assault
- Diploma in Medical jurisprudence
- Diploma in the History of medicine
- Diploma in GenitoUrinary medicine
- Diploma in the Philosophy of medicine
- Diploma in the Medical care of catastrophes
- Diploma in the Forensic medical sciences
- Diploma in HIV medicine
In the early 1800s the practice of medicine was plagued by charlatans:
unskilled people claiming to be doctors. Those who were trained took
umbrage at this situation and sought to remedy it. The College of
Physicians, the College of Surgeons and the Society of Apothecaries met
to agree on a petition to the government. This resulted in the 1815
Apothecaries Act. The Act set down the requirements for registration as a
doctor. This includded an apprenticeship and training in anatomy,
botany, chemistry, materia medica and "physic" (medicine). This act was
the beginning of regulation of the medical profession in England. Up to
this point a doctor ccould be someone with formal medical education
through the university of Oxford or Cambridge or it could mean someone
who had been apprenticed to an apothecary.
Australia's First Doctor
The first European doctor to set foot in Australia was Frans Jansz, who was the ship's surgeon on the Dutch ship Batavia. He came also with his assistant surgeon Aris Jansz. Their ship was the pride of the Dutch East India Company and was on its maiden voyage when it was shipwrecked on Houtman Abrolhos in 1629 (about 40km west of the area now known as Geraldton). Amongst the 220 survivors was another medical practitioner, Jeronimus Cornelisz, an apothecary. He took charge of the survivors whilst the ship's commander, Francisco Pelsaert, sailed in a longboat to the east to the Western Australian coast. Here he sought to find water, but having found none, proceeded to sail north to Jakarta, where he was supplied with a rescue ship. In the 15 weeks that Pelsaert was away, Cornelisz organised a band of mutineers who brutally murdered all but 80 of the survivors, including most of the children and women. The executions and rapes that occured make it the worst page in Australian history. Frans Jansz was amongst the many who were murdered by Cornelisz's mutineers.
A further account can be found here.
The Convict Era
The First Fleet
The First Fleet consisted of 11 ships that left
Great Britain on 13th May 1787 to arive in Botany Bay in 18th January
1788, having sailed 251 days. The fleet consisted of two Royal Navy
vessels, three store ships and six convict transports, carrying more
than 1,000 convicts, marines and seamen. It had stops in Santa Cruz at
Tenerife, Rio de Janeiro and Cape Town. This was one of the world's
greatest sea voyage, 1,487 people in total traveling 24,000 km. There
were 48 deaths on the journey (~3%). There were 10 doctors on the 11
ships. The diary of Mr Arthur Bowes Smyth (who was one of the 10) still exists and gives a good account of life on the voyage. The doctors had to deal with all the medical problems for the
journey. The following stayed in Australia to support the new colony;
- Assistant Surgeons
- Balmain
- Arndell
- Considen
- John Irving
Over the total peiod of transportation, about 350 doctors mage the
voyage to Australia (and back for many). Some more than once. Also, 112
doctors arrived as convicts (of the 160,000 people transported as
convicts)7
A hospital was established by Principal Surgeon John White.
1788 - Some scurvy occured amonst the convicts
1789 - 7th September, Governor Phillip was speared in the shoulder by an aboriginal person, whilstthe Governor was in the Manly area. He was treated successfully by Surgeon Balmain.
An pox-like disease (most likely smallpox) infected the local Aboriginal people with numerous subsequent deaths. The origin of this disease has never been established but logiaclly can only have come from the British or the French who landed in Botany Bay only weeks after the British arrived.
The Second Fleet
| Medically the second fleet was a disaster compared to the first.
The contracted shipping company was paid for every convict accepted, not
delivered. In fact there was a perverse incentive to have the convicts
die along the way.... it meant that they could also sell the provisions
not used. Of the 939 male convicts and 78 females embarked, and only
692 males and 67 females landed at Port Jackson. This meant that 759 of the 1017
convicts arrived alive: of these 500 were sick and/or dying. The second
fleet brought with it a portable military hospital. The medical sevices
were overwhelmed. What was worse was that the new colony had been starving and were of great expectation that the second fleet would bring food and supplies. One of the supply ships had been lost at sea and so the second fleet arrived without enough provisions.
Surgeons John Harris and D'Arcy Wentworth arrived on the seconfd fleet. John White stayed untl 1794.
1796 - William Balmain became Principal Surgeon.
1803 - Surgeon Mountgarret becomes the doctor for the new colony on the Derwent River in Van Diemen's Land.
1804 - Vaccinations for smallpox are commenced in Sydney.
1804 - Surgeon Jamison is appointed Principal Surgeon.
1806 Governor Bligh removes the right of private practice from all Colonial Medical Service surgeons. He changes some of Jamison's medical appointments.
1808 - Jamison instigates a certification program for Australian doctors.
1810 - Governor Macquarie restores the right of private practice to doctors working for the Colonial Medical Service.
1811 - The first asylum for the mentally ill was established at Castle Hill in Sydney.
D'Arcy Wentworth becomes the Principal Surgeon.
|
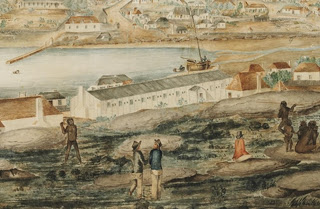 Courtesy of Mitchell Library
Courtesy of Mitchell Library |
Some Early Doctors
First doctors in the colony were the ships' surgeons (in the navy or
army) but were not always qualified. Over time, more doctors came, many
earning their passage by working as the ship doctor. There was little
scope for private practice in the early days medical services were
provided by the Colonial Medical Service. It initially consisted of five
doctors for the colony. They were to primarily treat the military and
the convicts. They were employed directly by the government (British
Treasury) and worked in tents. There were very few free settlers at this
time. Population health (quarantine and smallpox vaccination) was
organised by the various governors.
1788 - John White (1750 - 1832) was the principal surgeon for the first
fleet. He had served as a surgeon's third mate from 1778 and was
promoted to surgeon in 1780. In 1787 he joined the First Fleet at
Plymouth and traveled to the new colony of NSW on the Charlotte.
In 1788 he was appointed as Surgeon General for NSW. Within a week of
the arrival in Port Jackson, he and his team had to deal with scurvy and
an outbreak of dysentry. The lack of medical supplies encouraged him to
explore the native flora as a source and in 1788 was distilling
eucalyptus oil. He wrote A Journal of a Voyage to New South Wales (1790), in which he described many Australian species for the first time. White disliked Australia and returned to England in 1794.
1788 - Arthur Bowes Smyth (1750-1790), surgeon, was born on 23 August 1750 at Tolleshunt. He served on the Lady Penrhyn. His voyage was recorded in great detail in his diary, Journal of Arthur Bowes Smyth, 1787 March 22-1789 which is a rich source of information on the life aboard one of these convict ships.
|
1790 - D'Arcy Wentworth (1762-1827) came voluntarily to Botany Bay in 1790 on the second fleet ship, the Neptune
as the assistant surgeon. Having been born in Northern Ireland, he
attended medical school in London. He was accused of highway robbery,
and although he was not found guilty, he was advised to leave. Upon
arrival he worked for four years at Norfolk Island. He then moved to
Sydney, where Governor Lachlan Macquarie made him Chief of Police and
Treasurer of the Police Fund. From 1809 - 1817 he was the Principal
Surgeon. Wentworth gained considerable wealth from the contract to build
the Sydney Hospital. The contract gave the sole rights to import rum to
the colony. Consequently the hospital was called the Rum Hospital.
|
 |
"As a medical practitioner, Mr. Wentworth was distinguished for the
tenderness with which he treated his patients of every degree, and
especially that class of unfortunate persons whom the charge of the
General Hospital placed so extensively under his care. He was peculiarly
skilful in treating the diseases of children"9.
He became a founding director and major shareholder of the Bank of NSW. Wentworth died at his property Homebush
in 1827. The Sydney suburbs Homebush and Wentworthville derive their
names from his property and his name. His son, WC Wentworth, became
famous for his exploration and his work as a colonial lawyer, helping to
shape the early laws of Australia.
 |
1801 - William Redfern (1774 - 1833) was sentenced to death for mutiny,
but his sentence was commuted to life imprisonment. He had trained as a
surgeon's apprentice under his older brother and passed the
examinations of the London Company of Surgeons in 1797. He became a
surgeon's mate in the navy. He was transported in 1801 after four years
in gaol was and given a conditional pardon on arrival in Sydney. He was
transferred to work on Norfolk Island as an assistant surgeon. Although
he received a full pardon in 1803 he remained until 1808 at which time
he was appointed as an assistant surgeon at the new Sydney Hospital. He
resigned from the Colonial Medical Service in 1819 and developed a large
private practice. He became a founding member of the Bank of NSW. The
suburb of Redfern is named after him. Further information here.
|
1813 - The first Australian medical student, James Shears was
apprenticed to William Redfern. Following his death a year later, Henry
Cowper, aged 14, took his place. Medical training in the early colonial
period, usually consisted of apprenticeship to a doctor followed by
going to England for further training and examinations.
1814 - Dr William Bland arrived in Australia. He was sentenced to seven
years transportation for killing a ship's purser in a dual, whilst
working as a naval surgeon.
Dr William Redfern is commissioned by Governor macquarie to look into the high mortality of convict transportation (The Redfern Report). His report recommends various changes which reduce the convict deaths on the transportation ships.
1815 - In England, the Apothecaries' Act of 1815 was passed. This gave
the Society of Apothecaries the right to hold examinations and grant
licences to practice medicne. At this point in time in England there
were three groups of medical practitioners:
- physicians
- surgeons
- apothecaries (who became, over time, general practitioners!)
Membership of the Society of Apothecaries, at this time, required a
five year apprenticeship and then a viva voce examination (to which,
later, a written examination was added).
However, there were numerous other groups vying to treat the sick and
injured. These included barbers, quacks, druggists, chemists,
unqualified persons and vendors of empirical remedies. The druggists and
chemists eventually formulated their own body and became the
Pharmaceutical Society of Great Btitain.
1815 - Dr William Bland was given a pardon by Gov. Macquarie and offered an appointment as an assistant surgeon. He declined because it meant he had to appear before the Medical Assessment Committee. Instead he took up the position of Honorary Surgeon at the Castle Hill
Lunatic Assylum and the Sydney Dispensary. He set up as the first Australian doctor in full-time private practice.
The Military Hospital was built on Observatory Hill in Sydney.
1816 - Dr Willaim Bland starts teaching a medical student, William Sherwin.
The Sydney Hospital was set up. It was called the Rum Hospital because it was parlty paid for by a contract that allowed the exclusive imortation of rum.
1819- Dr James Bowman is appointed as Principal Surgeon. William Redfern, the senior assistant surgeon, who had been promised the position, resigned and set up as a private practitioner.
1820 - An influenza epidemic swept through the colony, killing large numbers of Aboriginal people and many of the young colonists.
The first private dispensary (pharmacy) was opened by John Tawell (an ex-convict) in Hunter St, Sydney.
1822 - Australia's first medical student to complete his training, Henry Cowper, obtained his MRCS in London. He had originally arived in Australia as an 8 year old child.
1823 - William Sherwin, who had been apprenticed to Mr W Bland, gains his MRCS in London. He is the first Australian born doctor to gain overseas qualifications.
1824 - The first hospital is built in the colony of Moreton Bay.
1826 - Dr Isaac Scott Nind arrives in Albany, Western Australia to become the western colony's first resident doctor.
An influenza epidemic in Sydney kills 37 people.
1827 - Andrew Gibson performed the first major elective surgery in Australia by ligating the femoral artery for an aneurysm.
1827 - The Sydney Dispensary is set up to provide outpatient care to the
poor. It is financed by charitable subscriptions and donations. It
later became the first public hospital in Australia: Sydney Hospital.
1829 - Dr Alexander Collie set up a tent hospital on Garden Island at the muth of the Swan River in WA.
The Later Colonial Era
Note that doctors in this era often had considerable interests outside of medicine, including political careers and farming.
The 1830s
1831 - the first friendly society was set up by boat builders to provide health insurance.
1832 - The British Medical Association was founded in England
1834 - There was an epidemic of measles
1835 - The government subsidised the Sydney Dispensary on a pound for pund basis.
1838 - The NSW Medical Board was formed via an act of parliament (2 Vic., Act No. XXII): 'An
Act to define the qualifications of Medical Witnesses at Coroner's
Inquests and Inquiries held before Justices of the Peace in the Colony
of New South Wales'. The Act states that:
- A coroner or justice of the peace (JP) can call upon the nearest
practicing, registered medical practitioner to attend a coroner's
inquest or JP's inquiry.
- For this to happen, there had to be a register of qualified practioners.
- Those to be admitted would be those doctors who had either:
- a Bachelor of Medicine of some university or
- a physician or surgeon licensed by or admitted into a college of physicians or surgeons in Great Britain or
- a member of the Comany of Apothecaries in London or
- a Medical Officer "duly appointed and confirmed by Her Majesty's sea or land service".
- The Governor may appoint a board of not fewer than three
members of the medical profession to be the NSW Medical Board. They
shall examine the qualifications of the applicants to the medical
register
- The Medical Board of NSW shall keep a written register of the qualified medical professionals.
1839 - The Deputy Inspector General of Hospitals intoduced a new system
of medical administration. The Colonial Surgeons submit their
resignations in protest. These are not accepted so as to avoid paying
retirement allowances.
The 1840s
The running of convict hospitals was given to local trustees. Doctors
worked in an honorary position. Few hospitals charged fees. Many small
privately owned hospitals started to appear, funded by subscriptions and
government subsidies.
1840 - R P Welch published the first Australian Medical Textbook, A Familiar Treatise on the Diseases of the Eye.
1842 - The Medical Register was commenced in Victoria in Port Phillip.
1844 - The Medico-Chirurgical Association of Australia was formed by Dr William Bland and colleagues.
1846 - Port Phillip Medical Association (PPMA) was formed by 12 doctors. The objectives were to develop a code of ethics, meet to discuss scientific papers, set up a library and publish a journal. The formulation of the code of ethics was divisive. The Australian Medical Journal was published but lasted only 6 months.
1847 - Mr Colin Buchanan performs (probably) the first major surgery under anaesthetic in Australia.
The 1850s
Most doctors are now working privately on a fee-for-service basis and
seeing those who could not afford to pay, for free. Some had otherforms
of income eg contracts with the benevolent societies, or capitation fees
for registered patients.
In 1852 some of the PPMA members helped form the Victoria Medical
Association (VMA).
1850 - There are 284 registered doctors in NSW.
1852 - Andrew Bosisto, a pharmacist, started the commercial production of eucalyptus oil (?the beginning of a pharmaceutical industry in Australia)
1853 - The Medical-Chirurgical Association of Victoria was formed.
1853 - The Castlemaine Medical Association was established
1853 - Another epidemic of measles
1854 - Mt Alexander Medical Association
1854 - Bendigo District Medical Association
1855 - The Victoria Medical Association and the Medical-Chirurgical
Association of Victoria were amalgamated to form the Medical Society of
Victoria (MSV)
1855 - The NSW Medical Registration Act required applicants to the Medical Register to have at least three years study.
1856 - The Australian Medical Journal re-commences in Melbourne and runs until 1914.
1857 - The Sisters of Charity opened St Vincent's Hospital in Sydney
1857 - Certification of death becomes a requirement in NSW/.
1857 - In England a committee formed to draw up "a nomenclature of
diseases to be used in the military services and in civil life". Members
of the committee were drawn from the College of Physicians, the Society
of Apothecaries, the College of Surgeons, the Registrar General, and
the medical departments of the army, navy and the East India Company.
(?the first standardised medical classification system?)
1858 - The The British Medical Act established a single register for all
medical practitioners and determined the qualifications that were
acceptable and who could work in hospitals. This register extended to
all the British colonies.
1858 - England. The curriculum for the medical studies (the Society of
Apothecaries) included examinations in the following subjects; anatomy,
physiology, chemistry, practical chemistry, botany, materia medica, the
Latin of the Pharmacopoeia, prescription, principles and practice of
medicine, midwifery (including the diseases of women and children),
forensic medicine, toxicology and morbid anatomy6
1859 - The Australian Medical Association is formed in Sydney by Dr William Bland. It lasts until 1869.
The 1860s
1860 - Another epidemic of measles
1861 - Dr George Pringle MD pioneered the use of Lister's antisepsis principles in Parramatta, NSW
1862 - Melbourne University established the first medical school.
1864 - There are 335 registered medical practitioners in Victoria.
1867 - Another epidemic of measles
1868 - The Medical Association of Victoria (MAV) was formed. It published The Australian Medical Gazette
At about this time a brach of the British Medical Association (BMA) was
formed in Victoria with about 30 members. This worked together with the
MSV for a while, with the MSV's activities focussing on the science of
medicine and the BMA on meico=political issues and ethics. The two
organisations were plagued with dissent and in-fighting to the point of
resignation of Council.
The 1870s
1874 - The Compulsory Vaccination Act in Victoria is passed. All
children were required to be vaccinated against smallpox by six months
of age.
1875 - The Australian Health Society began in Melbourne. Its focus was
on public health.
1875 - Sixty medical practitioners petition the NSW Legislative Assembly
for a determination to self-regulate the profession. This entailed:
- the ability to accept or decline membership in order to reject those of infamous conduct
- the ability to deal with imposters
- recognitions of doctors who had achieved their status through significant study
The 1880s
Compulsory notifications of infectios diseases begins.
Immigrants with specialist medical/surgical qualifications arrive in lager numbers.
1880 - The Australaian Medical Gazette commenced in Sydney and ran until 1914.
1881 - There are 454 registered medical practitioners in Victoria (after the gold rush).
1883 - Sydney University's Medical School begins.
1885 - THe first female medical student in Australia is enrolled at Sydney University.
1885 - Adelaide's medical school begins.
1886 - England. To become a registered medical practitioner one needed
to qulaify in medicine, surgery and midwifery. This could be obtained
through the University of London, the College or Physicians, the College
of Surgeons or the Sociaety of Apothecaries of London. Candidates would
qualify in either medicine or surgery6. The curriculum is five years. The exams are as follows:
- Primary part 1 - biology, physics, chemistry,materia medica, pharmacy
- Primary part 2 - anatomy, physiology, histology
- Final -
- Section 1 part 1 - principles and practice of surgery, etc (written and oral)
- Section 1 part 2 - principles and practice of medicine, etc forensic medicine, etc (written and oral)
- Section 1 part 3 - midwifery, gynaecology, etc
- Section 2 part 1 - clinical surgery
- Section 2 part 2 - clinical medicine and medical anatomy
Successful candidates were able to stlye themselves LSA (Licenciate of
the Society of Apothecaries) and would also receive a certificate in
dispensing.
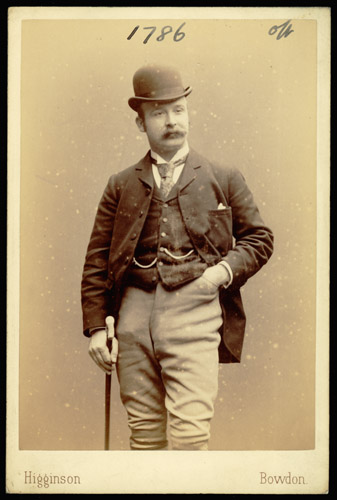 |
1889 - Doctors are required to have their photographs taken as part of their registration.
This requirement persists until 19275
Dr Walter Wignall's registration photograph, 1892. The reverse is stamped with the NSW Medical Board's stamp and the date.
Picture courtesy of and © State of New South Wales through the State Records Authority of NSW 2016
|
The 1890s
Australia entered into a depression.
Age and invalid pensions were introduced.
1890- Joseph Bancroft, a Brisbane doctor, discovered the parasite that cause filariasis
1891 - Melbourne University succeeds in having its MB BS recognised as a valid medical degree in England.
1890 - Dr Constance Stone became the first registered woman doctor in Australia.
1892 - There are 691 registered doctors in NSW.
1896 - The Medical Benevolent Fund of New South Wales is formed "to
afford assistance to any duly qualified medical man, widow or orphan
children of such, whom the Committee deem worthy of assistance.". It
continues until 1934.
1896 - The Queen Victoria Memorial Hospital was established by the three
sisters, Drs Constance, Clara and Mary Stone for treating women and
children.
1896 - Xrays are demonstrated in Australia
1899 - The NSW Royal Commission on Public Charities examined the running
of agencies receiving government subsidies. A recommendation was that
all hosptials should be placed under governmenr supervision and work
under licence.
The 1900s
1900 - The Medical Practitioners (Amendment) Act 1900 (Act No. 33, 1900)
was passed. It imposed penalties on persons using titles including
Surgeon or Physician if they were not appropriately registered.
1900 - The idea that the plague was transmitted by fleas from rats was put to practical demonstration by Frank Tidswell and J. Ashburton Thompson (of the NSW MEdeical Board). They controlled the epidemic by eradicating rats rather than by quarantine.
The Federation Era
1906 - The MSV and the branch of the BMA merged to become the Victorian branch of the BMA.
1908 - Legislation is passed to enable the Commonwealth government to provide care for those who cannot afford it.
1908 - 13th November, Frank Tudor (Labor) became responsible for health under the title of Minister for Trade and Customs. His term ended on 2nd June 1909
1908 - 2nd June, Robert Best (Commonwealth Liberal) became s responsible for health under the title of Minister for Trade and Customs. His term ended on 29th April 1910
The 1910s
1910 - 29th April, Frank Tudor (Labor) became responsible for health under the title of Minister for Trade and Customs. His term ended on 24th June 1913
1913 - 24th June Littleton Groom (Commonwealth Liberal) became s responsible for health under the title of Minister for Trade and Customs. His term ended on 17th September 1914.
1914 - 17th September, Frank Tudor (Labor) became responsible for health under the title of Minister for Trade and Customs. His term ended on27th October 1915, restarted with the new government and ended on 14th September 1916
1914 - The Australasian Medical Gazette in Sydney and the Australian Medical Journal (Intercolonial Medical Journal), in Melbourne merge into the Medical Journal of Australia
1916 - 14th September, Billy Hughes (Labor) became responsible for health under the title of Minister for Trade and Customs. His term ended on 14th November 1916
1916 - 14th November, William Archibald (National Labor) became responsible for health under the title of Minister for Trade and Customs. His term ended on 17th February 1917
1917 - 17th February, Jens Jensen (Nationalist) became responsible for health under the title of Minister for Trade and Customs. His term ended on 13th December 1918
1918 - 13th December, William Watt (Nationalist) became responsible for health under the title of Minister for Trade and Customs. His term ended on 17th January 1919
1919 - 17th January, Walter Massey-Greene, (Nationalist) became responsible for health initially under the title of Minister for Trade and Customs andlater under the title of Minister for Health. His term ended on 5th February 1923
 |
Surgery at the Children's Hospital, 1914
Picture courtesy of and © State of New South Wales through the State Records Authority of NSW 2016
|
The 1920s
The state governments are providing treatment to the poor for free through their hospitals. These hospitals are staffed by honorary medical officers, ie doctors who work for free for those who could not afford their fees. These doctors have private rooms and charged the more wealthy for their services. This meant that essentially the system worked because those who could afford treatment indirectly paid for those who could not. Such honorary positions carried some prestige and were generally well sought after.
|
Friendly Societies and Lodges
A gap existed between those who qualified for free treatment and those who could afford to pay the doctor's and the hospital's fees. Local groups banded together to form lodges or "friendly societies". Members contributed fees on a regular basis and the society or lodge paid for their medical treatment and/or funeral benefits when required. Variabilities in expenses from year to year made could threaten the viability of such insurance schemes. A way to offset this was to pass the risk "downstream", ie to the doctor. The societies had a fixed income and a known number of members. The sensible thing was to covert the costs into a fixed amount as much as possible. This was done by offering the doctors a fixed amount per year per patient to provide treatment (at no cost to the patient). There were advantages to the doctor for this capitation scheme. He had a steady income and this was particularly important for a young doctor first setting up. Also it meant that the doctor would receive some income for treating patients who previously had been unable to pay at all. Disadvantages included the failure of such schemes to renegotiate the docor's payments each year, resulting in increasing disenchantment. Doctors in any area became locked into these schemes because any doctor opting out would find his patients would leave and go to other doctors still in the scheme .
|
1923 - 9th February, Austin Chapman (Nationalist) became Minister for Health. His term ended on 26th May 1924
1924 - 26th May, Littleton Groom (Nationalist) became Minister for Health. His term ended on 13th June 1924
1924 - 13th June 1924, Herbert Pratten (Nationalist) became Minister for Health. His term ended on 16th January 1925
1925 - 16th January, Sir Neville Howes (Nationalist) became Minister for Health. His term ended on 22nd October 1929
1926 - A royal commission recommended a national insurance scheme to provide health insurance, maternity benefits, sickness benefits and superannuation. It was to be partly funded by employer contributions. The legislation failed to make it through parliament.
1926 - Dr Mark Lidwell from the Royal Prince Alfred Hospital, Sydney,
developed the first defibrillator
1926 - The Medical Benevolent Association of New South Wales is formed,
funded by the Medical Benevolent Fund of New South Wales.
1928 - Dr Mark Lidwill was first in the world to use cardiac pacing. He resuscitated a stillborn child at the Crown Stree Women's Hospital, using an insulated electrode inserted transcutaneously into the ventricular muscle.
1929 - 22nd October 1929, Frank Anstey (Labor) became Minister for Health. His term ended on 3rd March 1931
1928 - The Australian Inland Mission Aerial Medical Service began
in Cloncurry, Queensland (later renamed the Royal Flying Doctor Service)
due to the work of a Presbyterian minister, Reverend John Flynn.
Initial visits to remote areas were accomplished via a fabric covered
bi-plane, the Victory.
Photo: Patient from Camooweal, Queensland,
being unloaded from one of the early Royal Flying Doctor Service flights
in Brisbane, ca. 1930.
Picture courtesy of Trove, National Library of Australia
|

|

|
Later consultations were achieved using pedal powered radios in the
outback stations to communicate with the bases (telehealth!).
Photo: "A women is using a Traeger pedal
wireless while three children look on. The wireless has been set up
outside their house.
The invention of the pedal wireless in 1926 by Alfred Traeger brought a
significant change to life in remote places. This change was more far
reaching than providing help in emergency medical situations - it also
helped reduce the isolation and loneliness by enabling people who lived
hundreds of kilometres apart". Courtesy of the John Oxley Library, State Library of Queensland
|
The 1930s
Sulpha drugs became available
1931 - 3rd March, John McNeill (Labor) became Minister for Health. His term ended on 6th January 1932
1932 - 6th January, Charles Marr (United Australia) became the Health Minister. His term ended on 12th October 1934.
1932 - Edward Both produced the first portable ECG machine. This machine could also show the heart's activity as it occurred.
1934 - 12th October, Billy Hughes (United Australia) became the Health Minister. His term ended on 6th November 1935.
1934 - The Victorian Section of the Australian Aerial Medical Services (later the RFDS) started.
1935 - 6th November, Sir Earle Page (Country) became the Health Minister. His term ended on 7th November 1938
1936 - The Central Operations of the Australian Aerial Medical Services
(later the RFDS) is formed providing, in 1937, services to South
Australia and the Northern Territory.
1936 - The NSW Section of the Australian Aerial Medical Services (later the RFDS)was formed
1936 - The Western Australian Section of the Australian Aerial Medical Services (later the RFDS)was formed
1937 - The Eastern Goldfields Section of the Australian Aerial Medical Services (later the RFDS) was officially established
1938 - 7th November, Harry Foll (United Australia) became the Health Minister. His term ended on 26th April, 1939
1938 - 26th April, Sir Frederick Stewart (United Australia) became the Health Minister. His term ended on 14th March, 1940
1938 - Adelaide brothers Edward and Don Both develop an inexpensive cabinet to be used instead of the "iron lungs" for treating respiratory failure from polio.
The 1940s
Following graduation a small percentage of doctors would work in the hospital system; most would move into general practices for some years. Having experienced this type of work and found an area of specific interest, some would choose to re-enter the hospital system to train in a speciality. It meant that almost all doctors had an understanding of, and a respect for, gerneral practice. Most of these doctors ended up travelling overseas for their training (mostly to the UK). Once they had completed their training they would return and seek a hospital appointment, normally working as a junior honorary specialist in a teaching hospital.
In the post-war years, Australia's population grew at an increased rate. More hospitals were built, mostly in the cities, and hospital bed numbers increased. This enabled the establishment of Australian hospital based teaching for the specialities. With increasing numbers of specialists in hospitals came the reduction of general practitioners with admitting rights, particularly in the urban areas.
A young Australian doctor received a scholarship to study general practice in the UK. He visited 55 genral practices variously from rural, industrial and urban areas. He sat in on the consultations and home visits and observed the doctors at work. It is likely that he had little idea of the impact his observations would have. His name was Dr Joseph Silver Collings
For a description of what it was like to be a GP in the 1940s click here.
1940 - 14th March, Harold Thorby (Country) became the Health Minister. His term ended on 28th October, 1940
1940 - 28th October, Sir Frederick Stewart (United Australia) became the Health Minister. His term ended on 7th October, 1941
1941 - The National Health and Medical Research Council (NH&MRC)
proposed a national salaried medical service available to all. This was
opposed by the AMA. A subgroup of the NSW branch of the British Medical
Association was formed: the Sociological Section, in support of such a
scheme.
1941 - 7th October, Jack Holloway (United Australia) became the Health Minister. His term ended on 21st September, 1943
1942 - Penicillin became available, revolutionising the treatment of infections.
1943 - 21st September, James Fraser (Lab) became the Health Minister. His term ended on 18th June, 1946
1946 - The federal government (Labor) seeks to nationalise medicine along the lines of the British National Health Service.
1946 - 18th June, Nick McKenna (Labor) became the Health Minister. His term ended on 19th December, 1949
1948 - The Australian branch of the BMA successfully opposes the Chifley government’s National Health Act of 1948 in the High Court.
1949 - Professor John Cade, from Melbourne, publishes Lithium salts in the treatment of psychotic excitement in the MJA. This is one of the first instances of drugs used to successfuly treat mental illnesses.
1946 - 19th December, Sir Earle Page (Country) became the Health Minister. His term ended on 11th January 1956
The 1950s
More Australian based teaching positions for specialists became available. It became more common for a doctor to enter straight into a training program without first working in a community based general practice. Technology was improving and there were now many effective drugs. The specialists now became better at diagnosis and treatment of illness. Consequently their prestige and their incomes increased.
Increasing management of patients by specialists in hospital saw some decline in general practice. The prestige of general practice was reduced by the view that specialists had obtained further training and hence were beter. Also, any doctor who failed his specialist exams ended up in general practice.
Dr Collings published his findings in the Lancet. His comments were blunt. General practice in the UK was in a poor state, despite the hard work of conscientious doctors. The editor of the Lancet was fair in his comments about the paper. He warned that this report could not be ignored. He noted that Dr Collings, as an outsider was well-placed to make objective findings. Collings had seen general practice in Australia, New Zealand, Canada and the Uniterd States. Collings' article sent ripples throughout the UK medical establishment. Far from viewing themselves as the best in the world, they were now having to do something to improve their health care delivery. As a result, the British College of General Practitioners (BCGP) was formed in 1953. Its aim was to improve education and standards. The establishment of this new college was opposed by the three royal colleges (RCP, RCS, RCOG). The BCGP was not universally welcomed by GPs in the UK as it entailed further study and further costs.
Dr William Arnold Conolly was one of a small number of Australian GPs who were foundation members of the BCGP. He was instrumental in the formation of a NSW faculty of the BCGP. In 1952 a meeting was held at the home of Dr Warburton in Pymble, NSW for the purposes of forming a NSW faculty. A number of other state faculties were started across Australia.
- In 1954 the Queensland faculty is formed.
- In 1956 the WA and Vic faculties are formed
- In 1957 the Tas faculty is formed.
- In 1958 the SA faculty is formed
In 1953 the federal government (a liberal-Country Party coalition), with the blessing of the Australian branch of the BMA, launched the first national insurance scheme. Under this scheme, partly funded by taxpayers, private (not-for profit) insurance companies would provide rebates for medical services to fund members. Memebership was voluntary. Rebates for specialists were set at a level above those for general practioners, re-inforcing the idea that specialist consultations were of a greater value, however to access the specialist rebates, patients had to be referred by the GP. Under the same legislation, those patients recieving a Commonwealth pension would also have access to medical rebates through the Pensioner Medical Service. This meant that doctors treating pensioners in their rooms for free would now gain some re-inbursement. By the end of the 1950s most people (about 85%) belonged to a private (not for profit) health fund. Of the remainder, many received benefits via pensions or as war veterans.
In 1955 members from NSW, Qld, Tas and WA attend a meeting with the view
to establishing an Australian council. This was formed in November of the same year. Dr W A Conolly became the chairman and was later elected as president of the association at the first annual general meeting. In 1958 the states were amalgamated (with the support of the BCGP) to form the Australian College of General Practitioners. Conolly became the first president of the college and its office was first registered at his rooms in Cessnock, NSW. He became the first Fellow. The college established three committees; one for undergraduate education, one for post-graduate education and another for research.
1956 - 11th January , Donald Cameron (Liberal) became the Health Minister. His term ended on 22nd December, 1961
In 1959 the college appoints committees in the following areas:
- undergraduate education
- postgraduate education
- research
- preventive medicine
- publications
In ****** the Commonwealth government introduced the Pharmaceutical Benefits Scheme. This provided essential medications for free or at a subsidised rate.
Antihypertensive drugs become available.
For a description of what it was like to be a GP in the 1950s click here.
The 1960s
The Australian College of General Practitioners has to deal with membership issues. Should all general practitioners be allowed fellowship? If the College is to lift standards then fellows need to be a of a certain standard. The best way to guarantee this is to set an entrance exam. This proposal is not universally liked, but became the accepted route to fellowship. The College forms an association with the AMA; the College will focus on education and standards and the AMA will focus on advocacy and medico-political representation. When the government proposes univeral medical insurance, a common fee schedule is set. The amount for general practitioners is seen as inadequate by the College. In its first test of support for general practitioners, the AMA fails to be representative, supporting the fee schedulae against the wishes of the College.
New graduates are still able to obtain registration and move immediately into general practice (ie no inten year) in the early 1960s.
Neonatal intensive care units are established. Babies of 600g can now be kept alive.
For a description of what it was like to be a GP in the 1960s click here.
1960 - The first Australian General Practitioners’ Convention is held in Melbourne
1960 - The Tasmanian Section of the Royal Flying Doctor Service (RFDS) is formed
1961 - One of the first grey-scale ultrasound picures of a foetus is
demonstrated by Australians George Kossoff and Dr William Garrett from
the Royal Hospital for Women, in Sydney
1961 - 2nd December, Harrie Wade (Country) became Health Minister. His term ended on 18th November, 1964
1961 - "The college became affiliated with the AMA at the AMA’s
invitation. This frees the college from medicopolitical problems,
allowing it to concentrate on its academic programs of education and
research."2
1962 - "Dr Patterson records widespread opposition in the college to the
idea of a college examination, an idea floated by the Medical Education
Committee."2
1962 - The BMA Branches of the Australian states and territories formally merged into the Australian Medical Association
1962 - The College designs a five year training course for new graduates and a training program for those who had reccently entered general practice. Participation was voluntary.
1963 - The first Practice Management Seminar is organised by Dr N E Carson at the Batman Inn.
1964 - 18th November, Reginal Swartz (Liberal) became Health Minister. His term ended on 26th January, 1966
1965 - Requirements for entry into the ACGP include a rotating
internship for two years, three years approved training in general
practice and a requirement to satisfy the Censor-in-Chief of proficiency
in general practice.
1966 - the NSW faculty recommend grading of professional priviledges re
hospital appointments "provided that the doctor agrees the rules of the
hospital and satisfies the Credentials Committee as to their integrity,
experience and proven competence". The NSW Health Commission creates a
Medical Appointments Advisory Committee for the purpose of approving
appointments, taking control away from the College.
1966 - 26th January, Jim Forbes (Liberal) became Health Minister. His term ended on 22nd March, 1971
1967 - the ACGP establishes an entrance examination via a trial examination in Melbourne.
1967 - A scheme for student attachments in general practice is set up.
1968 - The ACGP conducts its first open entrance examination.
1968 - The ALP Opposition manages to set up a Senate Select Committee On Medical and Hospital Costs
1968 - There Coalition set up a three man Committee of Inquiry into Health Insurance, chaired by Justice J A Nimmo. The Nimmo Committee of Inquiry into the Medical Benefits Scheme is
completed and states that the current system is too complicated and
recommended changes.
1968 - Health economists, Drs Scotton and Deeble, from the Melbourne Institute of Applied Economic and Social Reform, make proposals, which the ALP use as their basis for their stand on health reform for the 1969 election.
1968 - St Vincent Hospital performs Australia's first heart transplant.
1969 - the ACGP became the RACGP following the Queen's blessing.
1969 - As a result of the Nimmo Inquiry the government announces the concept of
a common fee and guaranteed to fund this amount minus $5. The common fee was meant to represent the median value of the most commonly charged fee for various consultations. Specialists' fees were set at a higher rate. At the time this may have seemed fair because the specialists spent many extra years of study and work at low pay rates and because honorary specialists were treating many of the poor patients for free. The governemt set a maximum gap fee for billing of $5. The gap for a standard consultation was 80c and for a home visit was $1.20. As a result of this proposal, GPs providing the same proceedure as specialists, were being paid less. This became a dis-incentive for GPs to perform proceedures and caused GPs to consider that their services had been devalued. With the devaluing of these services and the lowered prestige of general practice, fewer graduates would seek to train in general practice. With more specialists and the devalued incentives for GPs to perform proceedures, fewer GPs provided these services, resulting in fewere GPs training in areas such as anaesthetics, obstetrics and surgery. There was also a fear that the government was setting up a national health service by stealth.
1968-1969 The General Practitioners' Society of Australia was formed to oppose the government's national health insurance proposals.
The 1970s
A defining time for general practice. The term itself was under threat as the RACGP actively sought to introduce the terms "family medicine" and "family physician". These terms did not catch on. The terms were more commonly used in North America, but UK doctors, with whom the Australian doctors were more likely to identify, did not use these terms, despite seeing themselves as family physicians.
Total health expenditure almost tripled in the 10 years from 1961 to 1971 ($683M - $1.7B)
1970 - The RACGP members overwhelmingly decied the fee proposals as
inadequate and decided to campaign against it. The AMA, however,
supported the fee proposal. This difference in opinion caused a rift
between the AMA and the RACGP.
1971 - 22nd March, Ivor Greenwood (Liberal) became Health Minister. His term ended on 2nd August, 1971
1971 - The Hornsby Vocational Training Scheme commences. Seven JRMOs trained under a pilot scheme supervised by Dr A Himmelhoch, for the purpose of training and as a study for the college’s vocational training
ideas.
Public concerns regarding perceived wastages and inapropriate
prescribing resulted in the government setting up the Select Committee of
the House of Representatives Inquiry into Pharmaceutical Benefits. The
RACGP was able to demonstrate the appropriateness of GP prescribing. The Australian Prescriber was set up in response to the college's recommendation that an independant prescribers journal be formed.
1971 - The Annals of General Practice are replaced by the Australian Family Physician (AFP)
1971 - 2nd August, Sir Ken Anderson (Liberal) became Health Minister. His term ended on 5th December, 1972
1971 - Accreditation of teaching posts in family practices and hospitals commenced.
1971 - The Australian Capital Territory Sub-Faculty of the RACGP was formed.
1972 - The Labour Party wins the Federal election after a 23 year hiatus. It proposed radical changes to the health system funding and in particular proposed a national system of health insurance funded by a tax surcharge and by federsal government funding.
1972 - The issue of the common fee persisted. An inquiry was held (the
Mason Inquiry). The RACGP argued that a GP consultations range in
complexity and consequently four fee structures were adopted based on
consultation length.
Check ups at 6 weeks, 15–18 months and 8 years of age were recommended
by the RACGP's Preventive and Community Medicine Committee.
The first issue of Practice Management was released as a supplement of the AFP.
The World Organisation of Family Doctors (WONCA) was established.
1972 - Medical Practitioners (Amendment) Act 1972, was passed. It established a separate register of specialists
1972 - 5th December, Lance Barnard (Labor) became Health Minister. His term ended on 19th December, 1972
1972 - 19th December, Doug Everingham (Labor) became Minister for Health . His term ended on 11th November, 1975
1973 - Declaration of Singapore was signed between the RACGP, the RACS, the RACOG and the AMA.
1973 - The government announced its plans for a National Health Scheme. This was met with mixed opposition from the different RACGP faculties, with the result that the RACGP did not oppose the government's plans.
1973 - The AMA opposed the Labor Party's National Health Scheme proposal, seeing it as a form of nationalised medicine akin to the UK's system.
1973 - The RACGP ended its close affiliation with the AMA (amicably) due to the diverging directions of the two groups.
The General Practitioners Society of Australia sees this as a betrayal of the RACGP. The RACGP resolves not to be involved in political representation.
1973 - The CHECK Program was first published.
1973 - The government created the Hospitals and Health Services Commission.
1973 - The Family Medicine Program (FMP) began and had an inital funding of $1.1 million to launch the program. This was provided by the Interim Hospitals and Health Sercices Commission under the government's "Community Health Program". This funding was controversial as many doctors did not want to see the training of GPs as being a government provision. The objectives of the FMP were:
- To increase the standards of primary health care
- To involve family physicians and other members of the health team with community health care, education and research, on a regional baasis, thus reducing isolation.
- To educate teachers and ensure training posts met a suitable standard
- To develop suitable training resources
- To undertake research into community health issues.
To this list eas later added:
- To provide re-training for graduates who have been away from the practice of medicine for some time, eg women who have left to raise a family.
|
The General Practitioners Society of Australia (GPSA)
Formed in 1968 the GPSA was a right-wing organisation which aimed to represent GPs.
The GPSA opposed the introduction of universal health insurance, believing that it would destroy the rights of GPs. It opposed any part of government interferece with the delivery of private medical practice. It was particularly opposed to the idea of bulk-billing. The RACGP was seen by the GPSA in a bad light because of its acceptance of government money to provide GP training. The AMA was not left out of its firing line because the AMA accepted the government proposals in the form of Medibank.
NB the General Practitioners Society of Australia (GPSA) is not to be confused with the current GPSA (General Practitioner Supervisor Association), a completely different organisation.
|
1973 - The RACGP produced a prototype for medical record system.
1973 - A number of universities established Chairs of Community Medicine (General Practice).
1973 - The Doctors Reform Society of Australia (DRS) was formed because of concerns regarding Medibank3.
1973 - The government published its proposal of changes to the health system: "A Community Health Program for Australia".
1974
The Family Medicine Program (FMP) commenced and 238 trainees were enrolled.
Entry to the FRACGP was determined to be via the examination pathway.
The RACGP Health Record was published.
1975
the Ballarat Sub-Faculty of the RACGP was formed.
1975 - The government instigated its medical insurance reforms under the name "Medibank" on 1st July. The main principles were:
- medical and surgical benefits provided to all Australians
- 85% of the scheduled fee being paid for all consultations, investigations and procedures
- no limit was set on what doctors could charge for their services
- treatment in a public hospital was provided for free
- The Pharmaceutical Benefits Scheme was increased
- Direct billing of Medibank (at the 85% fee) was encouraged.
The initial funding by a 1.35% tax levy was rejected by the Senate and the whole scheme was funded by the government.
1975 - November. The Labor Party lost power and was replaced by a Liberal-National Party government. The new government instigated a review of Medibank and determined that it was not viable financially. Universal free hospital access was ceased in almost all hospitals in successive years. Free access was determined by means testing. Doctors could no longer direct bill the government except for pensioners and unemployed patients.
1975 - 11th November, Don Chipp (Liberal) became Minister for Health. His term ended on 22nd December, 1975
1975 - 22nd December, Ralph Hunt (National Country) became Minister for Health. His term ended on 8th December, 1979
1976 - The National Trainees Association is established.
The RACGP proposed to the AMA that general practice should be recognised as a speciality.
1977
The Manual of General Practice, a revised version of the New Zealand manual, was published
The Newcastle/Hunter Valley Sub-Faculty of the RACGP was formed with
close ties to the medical school at the University of Newcastle.
1978
The first RACGP Computer Conference was held in Jolimont, Vic.
The RACGP Medical Education Committee set up a sub-committee on rural
practice and holds a conference for rural doctors: "Country Towns, Country Doctors"
The RACOG's Joint Diploma in Obstetrics and Gynaecology was created.
1979 - Rural registered posts were created in Lismore, Dubbo, Orange and Wagga Wagga
1975 - 8th December, Micahel MacKellar (Liberal) became Minister for Health. His term ended on 20th April, 1982
The 1980s
Rural registrar training posts were no longer available.
Specialist skills training posts become unavailable due to opposition from specialists
The Formative Evaluation of the Family Medicine Program was published
The RACGP's Scope for General Practice and Training for General Practice was published
The RACGP's progressive trainee assessment began
The RACGP published Computer Systems for General Practice
A stream for training rural GPs within the RACGP commenced in SA
The RACGP published Computerised Medical Record Systems – Proposed Minimum Standards.
A Joint Diploma in Obstetrics became available (RACGP and RACOG) but was not initiated until 1982
1982 - 20th April, Peter Baume (Liberal) became Minister for Health. His term ended on 7th May, 1982
1983 - 7th May, Jim Carlton (Liberal) became Minister for Health. His term ended on 11th March 1983
1983 - 11th March, Neal Blewitt (Labor) became Minister for Health and later Minister for Community Services and Health. His term ended on 4th April, 1990
The 1990s
1990 - 4th April, Brian Howe (Labor) became Minister for Community Services and Health and later Minister for Health, Housing and Community Services. His term ended on 24th March, 1993
1992 - The Medical Practice Act 1992 repealed the 1838 Medical Act and all its amendments. The Medical Tribunal and a number of other disciplinary and review bodies were established.
1993 - 24th March, Graham Richardson (Labor) became Minister Health. His term ended on 25th March, 1994
1994 - 25th March, Carmen Lawrence (Labor) became Minister Human Services and Health. Her term ended on 11th March, 1996
1996 - 11th March, Micahel Wooldridge (Liberal) became Minister for Health and Family Services. His term ended on 26th November, 2001
The 2000s
2001 -26th November, Kay Patterson (Liberal) became Minister for Health and Aging. Her term ended on 7th October, 2003
2002 - The Medical Journal of Australia became available online
2003 - 7th October, Tony Abbott (Liberal) became Minister for Health and Aging. His term ended on 3rd December, 2007
2007 - 3rd December, Nicola Roxon (Labor) became Minister for Health and Aging. Her term ended on 11th December, 2011
2009 - 9th June, Warren Snowden (Labor) became Minister for Indigenous Health, Rural and Regional Health and Regional Services Delivery. This was later changed to minister for Indigenous health His term ended on 18th September 2013.
The 2010s
2011 - 11th December, Tanya Plibersek (Labor) became Minister for Health and Aging. Her term ended on 18th September, 2013
2012 - Revalidation begins in the UK. British doctors now have to prove they are fit to practice every 5 years. They are required to submit annual assessments.
2013 - On 18th September Senator the Hon. Fiona Nash became Minister for Rural Health
2013 - 18th September, Peter Dutton (Liberal National) became Minister for Health. His term ended on 23rd
December, 2014.
2014 - 23rd December, Susan Ley (Liberal) became Minister for Health and later the Minister for Health and Aging. She remains incumbent.
2016 - BMC Family Practice releases an article revealing British general practice is in crisis: revalidation being a major factor.
2016 - AHPRA releases its report on the process of revalidation of Australian Doctors.
2016 -  The Australian General Practice Alliance (AGPA) formed to represent the interests of general practice owners. The Australian General Practice Alliance (AGPA) formed to represent the interests of general practice owners.
References/Sources
1. Lewis, M.L., Medicine in colonial Australia, 1788–1900, Med J Aust 2014; 201 (1 Suppl).
2. Historical Timeline, RACGP website, accessed 4/3/2016
Siedlecky, S., Doctors Reform Society of Australia, WikiDoc, accessed 5/3/2016
4.
AMA - More than Just a Union, https://ama.com.au/article/more-just-union-history-ama accessed 9/3/2016
The Royal Flying Doctor Service history, https://www.flyingdoctor.org.au/about-the-rfds/history/ accessed 9/3/2016
Bennet, C., The Future of Clinical Practice, Medical Journal of Australia Centenary Dinner, Great Hall, University of Sydney, 4 July 2014. Online transcript accessed 9/3/2016
Leeder, S., MJA Centenary, Opening Address, The University of Sydney Great Hall, July 4th 2014, Online transcript accessed 9/3/2016
5.
Archives In Brief 72 - Records of the NSW Medical Board, NSW Government State Records
History of Medicine, Australian Acadamy of Medicine and Surgery, http://www.aams.org.au/contents.php?subdir=library/history/funding_prof_med_au/&filename=1788to1900, accessed 9/3/2016
6. Barrett, C.R.B., The History of the Society of Apothecaries of London, 1885
7. Australian Medical Pioneers Index
Barff, H. E., A Short Hisorical Account of the University of Sydney, Angus & Roberston, 1902
8.Transactions of the Associated Apothecaries and Surgeon-Apothecaries, ebook, accessed via Google Books, 12/3/2016
Ford, E., Australian Dictionary of Biography, Vol. 2, 1967
Convict Records
Hull, G., From convicts to founding fathers—three notable Sydney doctors, J R Soc Med. 2001 Jul; 94(7): 358–361.
9.
Wentworth, D'Arcy (1762–1827), Obituaries Australia
10.
General Practice in Australia,: 2000, The Office of the Medical Advisor, General Practice Branch, Canberra, May, 2000
11.
List of Australian Ministries, Wikipedia, accessed 20/8/2016: https://en.wikipedia.org/wiki/List_of_Australian_ministries
|